Antibiotic resistance refers to the ability of bacteria to withstand the effects of antibiotics, rendering these medications ineffective in treating infections they were once able to combat.
Antibiotics revolutionized modern medicine by enabling the effective treatment of bacterial infections. However, their misuse and overuse became a global heath threat that led to the emergence of antibiotic resistance. Antibiotic resistance occurs when bacteria evolve and adapt to withstand the effects of antibiotics which render these drugs ineffective in combating infections they were once able to treat. This phenomenon poses significant challenges to healthcare systems, potentially reversing the advancements made in medicine over the past century.
How Does Antibiotic Resistance Occur?
Antibiotic resistance is a natural evolutionary process in which bacteria develop mechanisms to withstand the effects of antibiotics. Bacteria being single-celled organisms, have the ability to adapt and evolve relatively quickly which allow them to survive in the presence of antibiotics. Here’s how antibiotic resistance occurs:

Genetic Mutation:
Bacteria reproduce rapidly and during this process genetic mutations can occur spontaneously. Sometimes these mutations affect the bacteria in a way that renders antibiotics ineffective against them. Mutations might alter the bacterial cell structure, enzymes or other components targeted by antibiotics. This process make them less susceptible or impervious to the drugs.
Natural Selection:
When antibiotics are introduced into an environment containing bacteria, susceptible bacteria are killed off while those with genetic mutations show resistance hence they survive and multiply. This selective pressure favors the survival of resistant strains. Over passage of time these resistant bacteria become dominant within the population.
Horizontal Gene Transfer:
Bacteria have the ability to share genetic material not only within their own species but also across different species. This transfer of genetic material can happen through processes like conjugation, transformation and transduction. Through these mechanisms bacteria can acquire genes that confer resistance from other bacteria even those of different species. This lead to rapid spreading of resistance traits among microbial communities.
Causes of Antibiotic Resistance
Antibiotic resistance is a complex issue influenced by various factors that contribute to the development and spread of resistance among bacteria. Some of the primary causes include:

Overuse and Misuse of Antibiotics:
- Inappropriate Prescribing: Antibiotics are often prescribed when they aren’t necessary such as for viral infections against which they have no effect. This overprescription contributes to the emergence of resistance.
- Incomplete Courses: Not completing the full prescribed course of antibiotics allows some bacteria to survive which potentially lead to the development of resistance.
- Self-Medication: Using leftover antibiotics or sharing them with others without proper medical guidance can also contribute to antibiotic resistance.
Use in Agriculture and Livestock:
Antibiotics are extensively used in agriculture for promoting growth and preventing diseases in livestock. This widespread use contributes to the development of resistant bacteria that can be transmitted to humans through food consumption or environmental exposure.
Lack of New Antibiotics:
There has been a slowdown in the development of new antibiotics due to scientific, regulatory and economic challenges. This lack of innovation limits treatment options and allows bacteria to evolve resistance faster than new drugs are developed.
Globalization and Travel:
The ease of travel allows resistant bacteria to spread across borders making it a global concern. Resistant strains can move between countries and continents through infected individuals, contaminated food or environmental sources.
Poor Infection Control Measures:
Inadequate sanitation, hygiene practices and infection control in healthcare settings contribute to the spread of resistant bacteria among patients leading to healthcare associated infections.
Environmental Factors:
Due to improper disposal of medications or agricultural runoff, antibiotics and resistant bacteria in the environment contribute to the selection and proliferation of resistant strains in various ecosystems.
Implications of Antibiotic Resistance
The implications of antibiotic resistance are far-reaching:

Increased Mortality and Morbidity:
Resistant infections are harder to treat and can lead to prolonged illness, increased hospitalization and higher mortality rate.
Threat to Medical Procedures:
Routine medical procedures like surgeries, chemotherapy and organ transplants become riskier when antibiotics are less effective in preventing and treating associated infections.
Economic Impact:
The economic burden of antibiotic resistance is substantial as it increases healthcare costs due to longer hospital stays, expensive treatments and lost productivity.
Combating Antibiotic Resistance
Addressing antibiotic resistance requires a multifaceted approach:
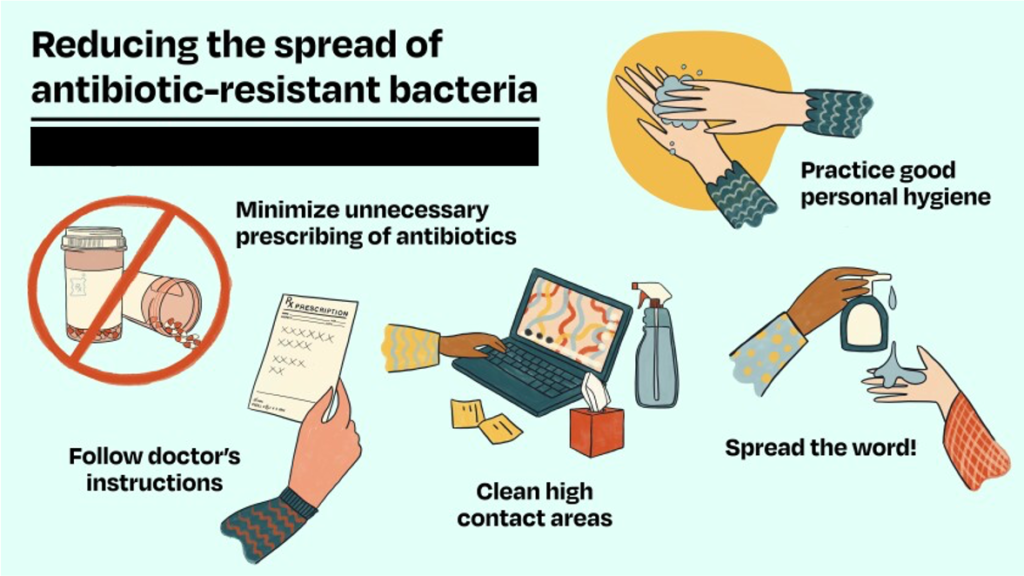
Responsible Antibiotic Use:
Promoting responsible use of antibiotics among healthcare providers, patients and in agriculture is crucial to slow down the development of resistance.
Surveillance and Research:
Enhanced surveillance of resistant strains and investing in research for new antibiotics and alternative treatment strategies are essential.
Global Cooperation:
International collaboration and coordination among countries are imperative to address the global nature of antibiotic resistance.
Conclusion
Antibiotic resistance is a complex issue threatening the effectiveness of the modern medicine. It demands immediate and coordinated action at local, national and global levels. Awareness regarding responsible antibiotic use, research into new treatments and global cooperation are essential to mitigate this escalating public health crisis and ensure the continued effectiveness of antibiotics in combating bacterial infections. Ultimately, safeguarding these invaluable medications for future generations requires concerted efforts from all stakeholders involved in healthcare, research and policymaking.
For more related news Click Here.

